The complex relationship between depression and sleep has long intrigued researchers and clinicians, serving as a fertile ground for exploration and discovery. By unraveling this intricate connection, we can gain invaluable insights that may lead to more effective treatment and management strategies for individuals suffering from these intertwined conditions. This article delves deep into the myriad of sleep patterns and disturbances that accompany depression, probing into the underlying mechanisms and reasons for their occurrence. Through a comprehensive examination of current research, we aim to shed light on this critical intersection, ultimately paving the way for enhanced therapeutic approaches and improved quality of life for those affected.
Is Sleeping On The Couch A Sign Of Depression?

For many people, the habit of sleeping on the couch might initially appear as a mere lack of convenience or a pursuit of casual comfort. However, when this behavior becomes habitual, it often raises deeper questions about an individual's mental and emotional wellbeing, potentially signaling conditions like depression. The link between sleeping on the couch and depression is increasingly recognized by mental health professionals, who suggest that this behavior may reflect an unconscious tendency to seek out new spaces for comfort or to escape the associations tied to traditional sleeping areas. This seemingly simple change in sleeping location can inadvertently become a poignant manifestation of an individual's internal struggle, where the couch emerges as a refuge that provides a temporary sense of solace. It allows one to disconnect from reality, symbolizing a retreat from daily life pressures and providing a safe space amidst emotional turmoil. This shift not only highlights the physical boundary one sets but also emphasizes the emotional distance that a person suffering from depression may experience, underscoring the need for understanding and addressing the underlying issues..
Exploring Sleep Apnea Secondary To Depression

The intricate interplay between sleep apnea and depression underscores the importance of recognizing and addressing coexisting conditions in clinical settings. When depression contributes to the development or worsening of sleep apnea, it often manifests through disruptions in sleep architecture, such as frequent awakenings and reduced REM sleep, which are critical for restorative rest. The bidirectional nature of this relationship means that the fatigue and cognitive impairments stemming from untreated sleep apnea can deepen the sense of hopelessness and fatigue commonly associated with depression, thus perpetuating a cycle of poor mental and physical health. Effective management requires a holistic approach, combining psychological interventions, such as cognitive behavioral therapy, with medical treatments like Continuous Positive Airway Pressure (CPAP) therapy to alleviate sleep apnea symptoms. By addressing both conditions concurrently, individuals may find relief and improvement in their overall quality of life, highlighting the necessity for integrative care strategies within mental health and sleep medicine disciplines..
The Connection Between REM Sleep And Depression

Rapid Eye Movement (REM) sleep is a critical phase of the sleep cycle associated with dreaming and memory consolidation. In individuals with depression, REM sleep is often disrupted, leading to what is known as REM sleep depression. People with depression may enter REM sleep more quickly and spend more time in this stage, which can impair the restorative functions of sleep. This disruption is not just a consequence of depression but can also aggravate the condition. Over time, the imbalance in REM sleep may exacerbate symptoms such as mood disturbances, cognitive impairments, and overall psychological distress. Additionally, the altered sleep architecture commonly observed in depression can affect the regulation of neurotransmitters and hormones that are crucial for emotional and mental well-being. Therapeutic interventions, such as cognitive-behavioral therapy for insomnia (CBT-I), have shown promise in helping to normalize sleep patterns, thereby potentially alleviating some symptoms of depression. However, ongoing research is needed to fully understand the bidirectional relationship between REM sleep and depression, and to develop more effective treatments that address both sleep disturbances and depressive symptoms simultaneously..
Understanding REM Sleep Depression
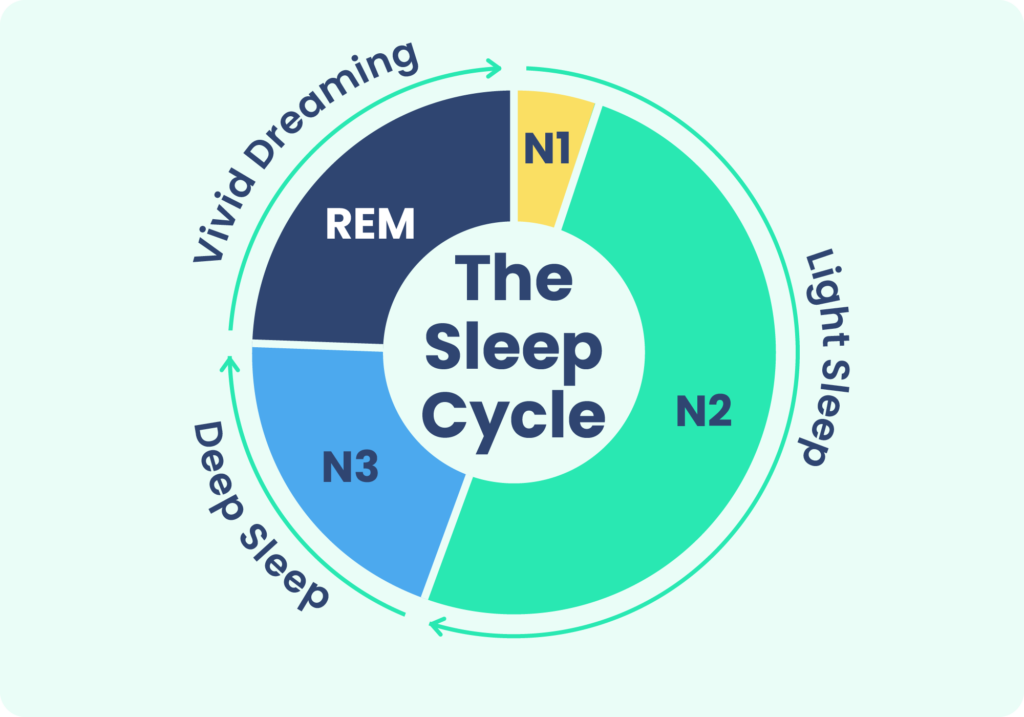
Recent studies have explored the neurobiological mechanisms underlying REM sleep depression, revealing a complex interplay between neurotransmitters like serotonin and norepinephrine, which are crucial for mood regulation and sleep architecture. The dysregulation of these neurotransmitters in depressed individuals disrupts normal sleep cycles, often leading to earlier onset of REM sleep and an increase in REM density—characteristics that are atypical in non-depressed populations. This aberrant REM sleep pattern not only impairs cognitive functioning and emotional resilience but also hinders the body's natural ability to process emotions and consolidate memories, thereby contributing to the persistence of depressive symptoms. Understanding these patterns has significant implications for developing targeted treatments, such as antidepressants that aim to normalize sleep architecture, or cognitive behavioral therapies designed to improve sleep hygiene and overall mental health..
The Role Of Sleep In Emotional Regulation

Enhancing sleep quality can therefore be a powerful tool in improving mental health outcomes. Sleep not only facilitates the consolidation of emotional memories but also aids in problem-solving and creative thinking, which are crucial for coping with life's challenges. In therapeutic settings, techniques such as cognitive-behavioral therapy for insomnia (CBT-I) are often employed to tackle sleep disorders, proving effective in alleviating depressive symptoms by re-establishing a healthy sleep cycle. Moreover, adopting good sleep hygiene practices—such as maintaining a consistent sleep schedule, creating a restful environment, and limiting exposure to screens before bedtime—can significantly benefit emotional resilience and cognitive clarity. By prioritizing sleep, individuals can better equip themselves to handle stress, reduce anxiety, and foster a more balanced emotional state, ultimately contributing to overall psychological well-being..
How Sleep Deprivation Impacts Depression
Chronic sleep deprivation not only exacerbates depressive symptoms but also carves a more intricate path toward cognitive and emotional disturbances. It has been observed that insufficient sleep distorts neurotransmitter activity within the brain, thereby disrupting normal brain functions and paving the way for mood disorders to take root. This disturbance in brain chemistry can lead to an increased vulnerability to depression, demonstrating a bidirectional relationship between sleep and mood. Furthermore, sleep deprivation may diminish the efficacy of antidepressant medications, underscoring the critical need for healthcare providers to systematically evaluate and address sleep issues as part of a comprehensive treatment strategy for depression. By prioritizing sleep health, we can enhance the overall well-being of individuals, ultimately leading to more favorable treatment outcomes and improving the quality of life for those affected by depressive disorders..
Treating Sleep Disturbances In Depressed Individuals
Incorporating a comprehensive approach to treating sleep disturbances in individuals suffering from depression is crucial for achieving optimal outcomes. Cognitive Behavioral Therapy for Insomnia (CBT-I) remains a cornerstone of this multifaceted strategy, as it directly targets the maladaptive thoughts and behaviors that contribute to sleep issues. By restructuring these negative thought patterns, CBT-I can effectively alleviate symptoms of insomnia and even mitigate the effects of sleep apnea often exacerbated by depressive disorders. In addition to CBT-I, pharmacotherapies such as sedative-hypnotics or melatonin agonists might be prescribed to help regulate the sleep-wake cycle. Moreover, lifestyle interventions like establishing a regular sleep schedule, engaging in physical activity, and reducing caffeine and alcohol intake play a vital role in promoting restorative sleep. Together, these interventions not only help improve sleep but also have the potential to enhance overall psychological well-being and reduce depressive symptoms..
The Importance Of A Comprehensive Treatment Plan

Moreover, integrating lifestyle modifications such as regular physical activity, a balanced diet, and mindfulness practices can further support the management of sleep and depression. Cognitive-behavioral therapy for insomnia (CBT-I) can be particularly effective in restructuring negative thought patterns and establishing healthier sleep routines. Additionally, ensuring adequate exposure to natural light during the day and maintaining a consistent sleep schedule can regulate the body's internal clock. It's also essential to create a supportive sleep environment by minimizing noise and distractions and promoting relaxation before bedtime. By addressing both psychological and physiological aspects, individuals can pave the way for a more restorative sleep experience and an improved overall mental well-being. Collaboration between healthcare providers, patients, and family members is key to tailoring these strategies effectively to each individual's needs, fostering long-term resilience against the cyclical nature of sleep disturbances and depression..
Future Directions In The Study of Depression and Sleep

This growing body of research highlights the intricate interplay between neurochemical pathways, mental health, and sleep regulation. As scientists delve deeper into the molecular level, they are exploring how genetic predispositions may influence the onset and severity of sleep issues among individuals with depression. Additionally, psychological factors, such as stress and maladaptive thought patterns, are being examined for their roles in exacerbating sleep disturbances. The hope is that by integrating genetic data with cognitive and behavioral analyses, clinicians can develop precision medicine approaches that tailor therapies to individual profiles. This personalized strategy holds promise for enhancing treatment efficacy, reducing side effects, and improving overall quality of life for those affected by both depression and sleep disorders..
In conclusion, the intricate relationship between depression and sleep underscores the critical need to integrate sleep health into depression treatment plans. By identifying and addressing sleep-related symptoms, such as habitual couch sleeping or disruptions in REM sleep, healthcare providers can intervene earlier and more effectively. This enhanced awareness and understanding pave the way for more holistic treatment approaches, ultimately leading to improved outcomes for patients. By prioritizing both mental health and sleep health, we can develop more comprehensive strategies that empower patients on their path to recovery and well-being.